News Release
Making masks smarter and safer against COVID-19
 |
January 21, 2021: A new tool for monitoring COVID-19 may one day be right under your nose. Researchers at the University of California San Diego are developing a color-changing test strip that can be stuck on a mask and used to detect SARS-CoV-2 in a person’s breath or saliva. (Read an updated FAQ with project leader and UC San Diego nanoengineering professor Jesse Jokerst on the Jacobs School blog.)
The project, which received $1.3 million from the National Institutes of Health, is aimed at providing simple, affordable and reliable surveillance for COVID-19 infections that can be done daily and easily implemented in resource-poor settings. It is part of the NIH’s Rapid Acceleration of Diagnostics Radical (RADx-rad) program for COVID-19.
“In many ways, masks are the perfect ‘wearable’ sensor for our current world,” said Jesse Jokerst, professor of nanoengineering at the UC San Diego Jacobs School of Engineering and lead principal investigator of the project. “We’re taking what many people are already wearing and repurposing them so we can quickly and easily identify new infections and protect vulnerable communities.”
The team will create test strips, or stickers, that can be put on any mask (N95, surgical or cloth). They will be designed to detect the presence of protein-cleaving molecules, called proteases, that are produced from infection with the SARS-CoV-2 virus.
 |
 |
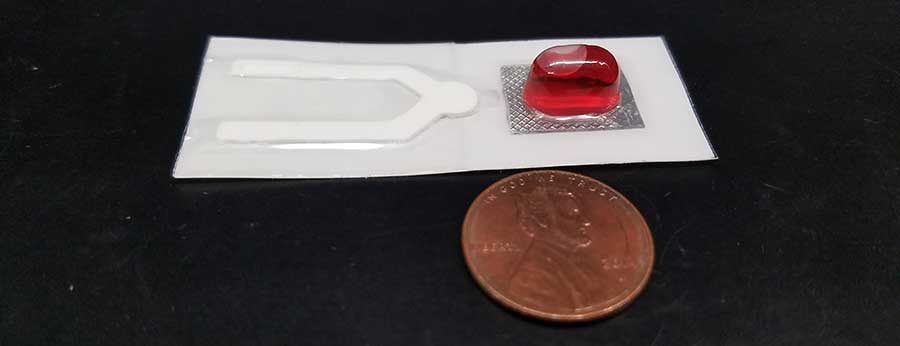
| Prototype test strip before use (top) and after use, showing a negative result (bottom). |
The idea is that as the user breathes through the mask, particles—including SARS-CoV-2 proteases if the user is infected—will accumulate in the test strip. At the end of the day or during a mask change, the user will conduct the test. The test strip is equipped with a blister pack that the user will squeeze, releasing nanoparticles that change color in the presence of the SARS-CoV-2 proteases. A control line on the test strip will show what a positive result should look like. It would be similar to checking the results of a home pregnancy test.
Jokerst notes that the strips are not meant to replace current COVID-19 testing protocols.
“Think of this as a surveillance approach, similar to having a smoke detector in your house,” he said. “This would just sit in the background every day and if it gets triggered, then you know there’s a problem and that’s when you would look into it with more sophisticated testing,”
 |
| Set of test strips. |
The test strips can be easily mass produced via roll-to-roll processing. This would keep costs down to a few cents per strip. “We want this to be affordable enough for daily testing,” Jokerst said. This would allow facilities at high risk such as group homes, prisons, dialysis clinics and homeless shelters to monitor for new infections earlier and more frequently to reduce spread, he said.
Jokerst is teaming up with researchers at UC San Diego School of Medicine to test the strips first on COVID-19-positive saliva samples, then on patients and healthcare workers at Veterans Affairs San Diego Healthcare System.
Co-investigators on the team are William Penny, professor of clinical medicine, and cardiologist at VA San Diego Healthcare System, Louise Laurent, professor of obstetrics, gynecology and reproductive sciences, and Rob Knight, professor of pediatrics, bioengineering and computer science and engineering, and director of the Center for Microbiome Innovation at UC San Diego.
Potential tool against future outbreaks
This technology can translate to future coronavirus outbreaks, Jokerst said. “The proteases we’re detecting here are the same ones present in infections with the original SARS virus from 2003 as well as the MERS virus, so it would not be too far of a stretch to imagine that we could still benefit from this work later on should future pandemics emerge.”
And even with vaccination efforts underway, this surveillance approach could be deployed in parts of the world where vaccines are not yet available or still limited in distribution.
Materials science approach to mask safety
In addition to this work, Jokerst and his team, in collaboration with UC San Diego nanoengineering professor Ying Shirley Meng, have conducted in-depth research on masks to answer a burning question that surfaced early on in the pandemic: Can N95 respirators be safely reused after being disinfected?
The answer, they found, is yes.
Since the start of the COVID-19 pandemic, health care workers have been facing shortages of personal protective equipment. Researchers and medical centers across the U.S. have found ways to decontaminate and reuse N95 respirators to help keep health care workers safe while serving on the front lines. Jokerst, Meng and colleagues wanted to explore exactly how safe and effective the respirators are for reuse.
A paper detailing this work was published in ACS Applied Materials & Interfaces. UC San Diego materials science Ph.D. student Wonjun Yim is the first author on the study.
| SEM images of the filter layer in an N95 respirator before heat treatment (left) and after (right). |
The UC San Diego researchers studied the materials science properties of N95 and KN95 respirators before and after decontamination—the process involved heating the respirators in an oven at 70 C (158 F) for 30 minutes at a time, three times total. They used a filtration apparatus to count how many particles in the air are captured by the respirators. They also examined the fibers of the respirators under an electron microscope.
The team discovered that after the heat treatment, the respirators were able to filter out 90 percent of airborne particles—a small drop from their original 95 rating. They also saw no changes in the structure, density or width of the fibers.
“These masks are more reusable than people think. This is good knowledge to have, to know that these still offer significant protection after being heated multiple times,” Jokerst said.
“People right now don’t understand what happens when you breathe on a piece of cloth all day,” he said. “These studies will lay the foundation to get us thinking about how we can use our masks in safer and smarter ways.”
Media Contacts
Liezel Labios
Jacobs School of Engineering
858-246-1124
llabios@ucsd.edu